Primary Care - Data
GPs
There are 11 GP Practices in Midlothian operating from 9 premises. A number of these premises are good quality and modern, the latest being Loanhead Medical Centre.
Demand for GP appointments is high. The average number of consultations is 6 per person per year (up from 3.7), and 600,000 appointments are offered every year. National figures suggest that 1 in 10 people visit their GP practice on a weekly basis (Public Health Scotland, 2023).
Between 84.6% to 98.9% people can access a GP within 48 hours or advance booking to an appropriate member of the GP team. NHS Lothian and Scotland rates are (93%) (Public Health Scotland, 2023).
The National Health and Care Experience Survey asks about people’s experiences of their GP practice and out–of-hours services, and their outcomes from NHS treatments. It is a postal survey which was sent to a random sample of people who were registered with a GP in Scotland asking about people’s experiences during the previous 12 months. The response rate for the 2022 results for Midlothian was 28% (Scotland’s return rate was 24%). This is lower than the previous 2 years.
Positive responses from patients about how they rate their GP has declined between 2016 and 2022.
- Midlothian responses dropped by 17% from 79% positive responses in 2016 to 62% in 2022.
- Scottish responses were higher than those in Midlothian, but have also dropped by 18% from 85% in 2016 to 67% in 2022.
In 2022, 62% of responses from Midlothian rated their GP Practice positively.
- 36% of people said their GP practice allows them to make an appointment more than 3 days in advance compared to 48% for Scotland.
- 88% of people said they had a positive experience when needing to see a GP urgently. This is lower than the previous result but similar to Scotland (85%).
- 86% of people who responded to the survey felt they were listened to by their GP practice. This is the same as Scotland (86%)
- 84% of people felt like they were treated with compassion and understanding (compared to 83% for Scotland)
(National Health and Care Experience Survey, 2022).
Prescribing
Prescribing data can give insights into the prevalence of illnesses requiring specific prescriptions. There are ongoing efforts of improvement around prescriptions. There is the development of HSCP led pharmacotherapy services to support GP workload and offer alternatives to encourage patient self-management of symptoms (where appropriate) through social prescribing such as green prescribing and fit-scriptions. Data collection around non-medical prescriptions is an area that can be difficult to measure but is developing.
Prescribed medication
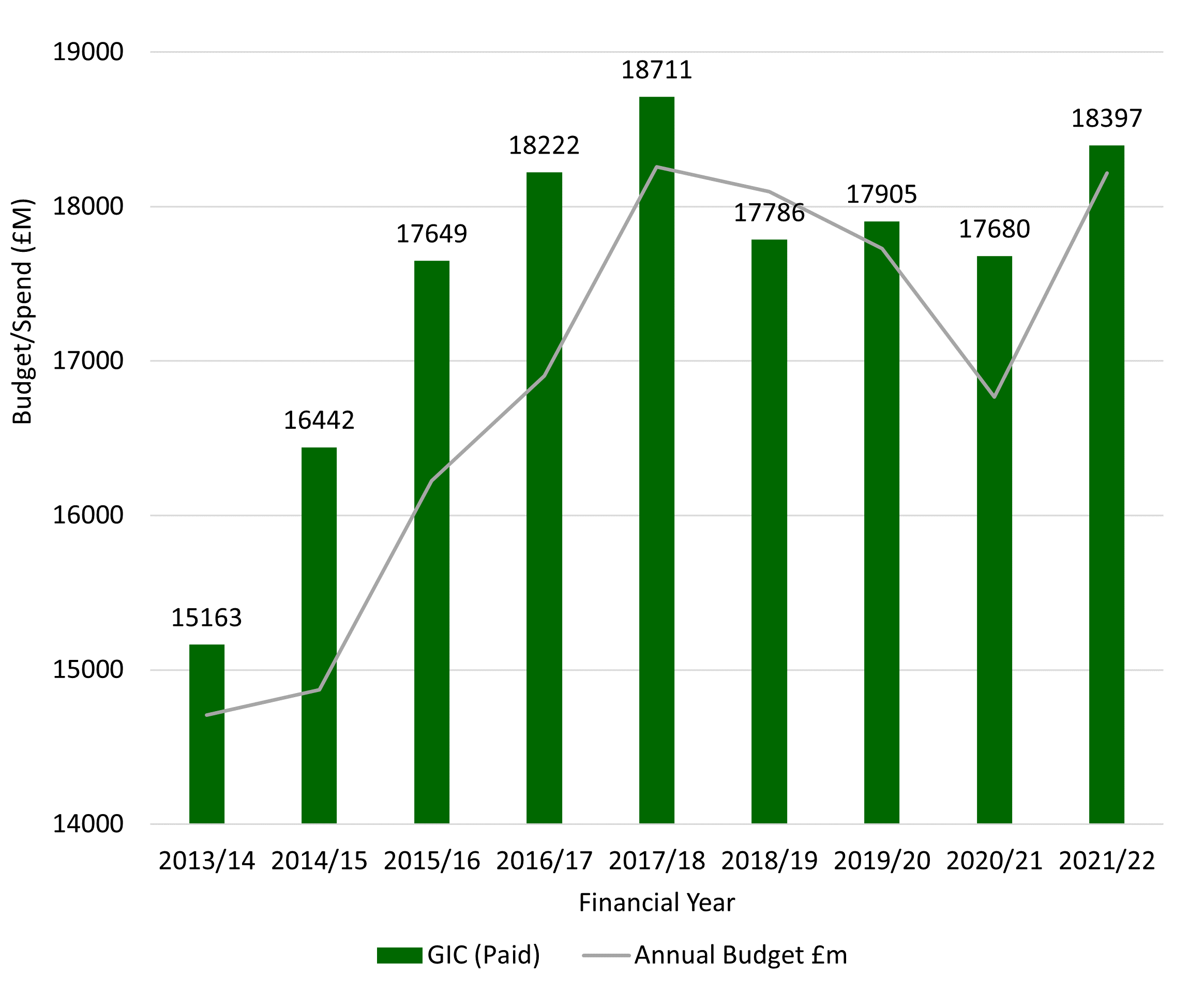
The continued increase in costs and associated challenges to maintain the allocated prescription budget has implications. The focus remains on reviewing areas of priority to improve health and reduce expenditure. Particular attention is required on those over 65 and those living in our more deprived communities. Regardless of savings made, the overall cost is expected to continue to increase (although at a lower rate). This is because of an ageing population and the fact that people are living longer with comorbidity.
Prescribing spend vs budget 2013/14 to 2021/22
Data source: NHS Lothian Internal Data: PRISMS
GIC refers to Gross Ingredient Cost. When we refer to spending on drugs, we use the paid gross ingredient cost (GIC). This is the cost of drugs to the NHS, excluding the fees paid to community pharmacists for drug dispensing and discounts.
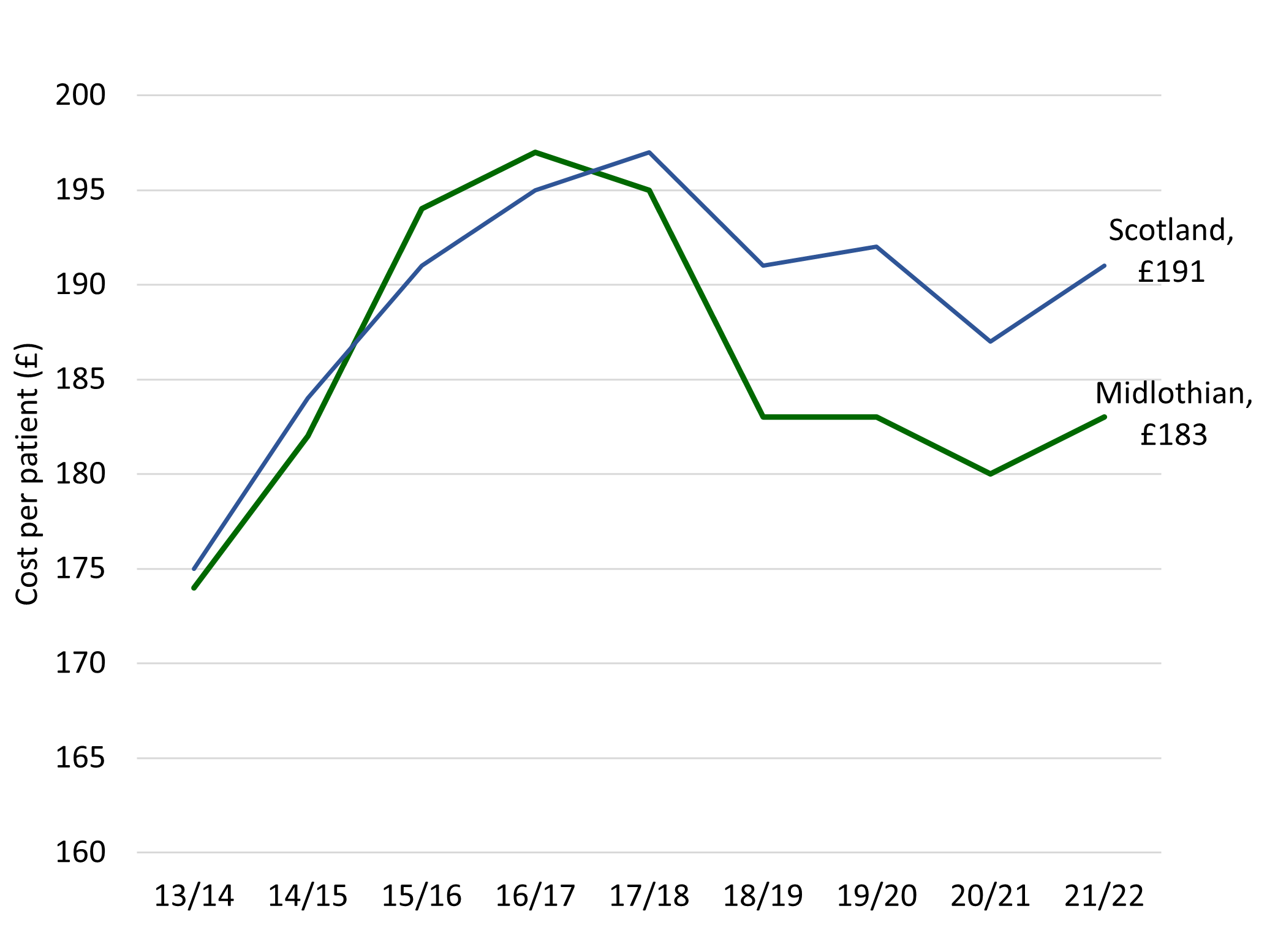
In 2021/22 £183 is the average GP prescribing cost per patient (2021/22), lower than a Scotland average of £191. In 2015/16 spending was higher than the Scottish average by £3 and was growing faster than the rest of Lothian and Scotland. Work has been done to reduce items prescribed and to support the policy of ‘realistic care, realistic medicine.’
The most frequently prescribed medicines in Midlothian in 2021/22 were:
- Atorvastatin (mainly for Heart problems)
- Omeprazole (mainly for indigestion and heartburn)
- Co-codamol (painkiller)
- Lansoprazole (mainly for indigestion and stomach ulcers)
- Levothyroxine sodium (thyroid problems)
The most expensive items in 2021/22 were:
- Apixaban (prevention of blood clots)
- FreeStyle Libre (diabetes monitor)
- Enteral nutrition (nutrition)
- Wound management dressings (dressings)
- Fostair (asthma inhaler)
Community Pharmacy
The community pharmacy contract aims to use the skills and knowledge of pharmacists better, ensuring that all patients have access to support in the management of their medicines as well as providing a minor ailments service for advice.
All pharmacies in Midlothian also now operate a NHS Pharmacy First Scotland service for people living in Scotland, those registered with a Scottish GP Practice, residents in care homes and care settings, people who are experiencing homelessness and gypsy travellers. The service allows community pharmacies to give people expert help for treating conditions such as sore throats, earache, and cold sores, along with common clinical conditions such as urinary tract infections. Pharmacy teams offer advice, treatment or referral to other healthcare teams if required. The service aims to help people access the right care in the right place, without having to go to their GP practice or local Accident and Emergency Department for non-urgent treatment.
Page updated October 2024.
